Abstract
Background Conventional chemotherapies have shown poor efficacy in patients with relapsed B-cell acute lymphoblastic leukemia (B-ALL) after allogeneic hematopoietic stem cell transplant (allo-HSCT). Chimeric antigen receptor (CAR) T-cell therapy has shown to be highly effective to achieve initial complete remission (CR) for B-ALL patients, even for these patients who relapsed after allo-HSCT but the duration of the remission needs to be much improved. For B-ALL patients who relapse post allo-HSCT, whether bridging into a second HSCT after CAR-T therapy can improve long-term survival remains controversial. We retrospectively analyzed long-term follow-up data on 97 B-ALL patients who relapsed after first transplantation and who have received CD19 or CD22 CAR-T therapy followed by consolidation second allo-HSCT to explore whether such a treatment sequence could result in better long-term survival.
Methods Between October 2015 and March 2022, 97 patients who received a consolidation second transplant post CAR-T therapy were retrospectively analyzed from 4 clinical trials registered at www.chictr.org.cn ChiCTR2000031340, ChiCTR-ONC-17012829
and www.clinicaltrials.gov NCT03173417, NCT04163575. The median follow-up time was 460 days (range: 33-1726 days) after the 2nd HSCT.
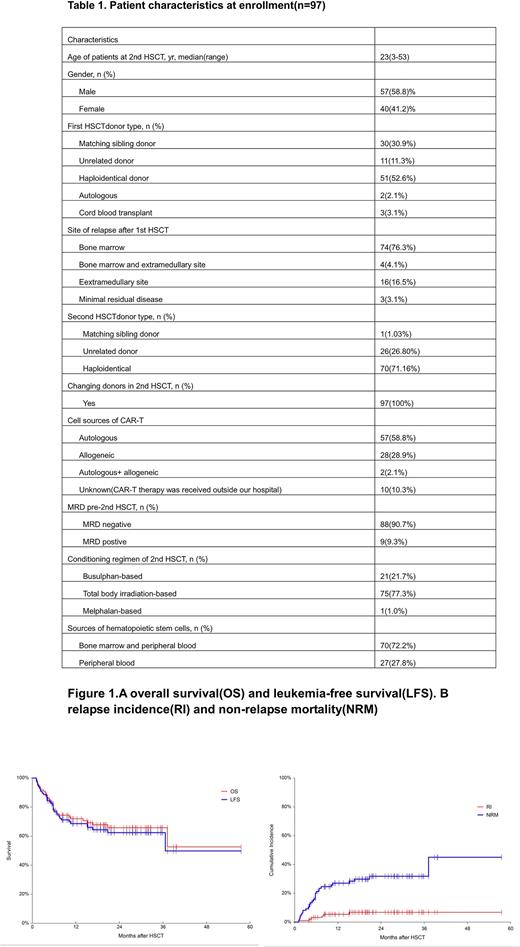
Results The median age of the patients was 23 years (range: 3-53 years). After the first transplant, 74 patients (76.3%) had a bone marrow relapse, 16 patients (16.5%) had extramedullary site relapse, 4 patients (4.1%) had both bone marrow and extramedullary site relapse and 3/97 patients (3.1%) had only positive minimal residual disease (MRD). Four patients received CAR-T therapy right after relapse. Ninety-three relapsed patients received chemotherapy, donor lymphocyte infusion (DLI) and other treatments before CAR-T therapy. Patients received autologous (n=57, 58.8%) or allogeneic CAR-T (n=28, 28.9%), and two patients (2.1%) received both autologous and allogeneic CAR-T. Detailed patient characteristics are shown in Table 1. The sources of CAR-T cells in the other 10 patients (10.3%) were unknown (CAR-T therapy was received outside our hospital). Following CAR-T therapy, all patients achieved CR. Prior to their 2nd HSCT, 88 patients (90.7%) were MRD-negative, and 9 (9.3%) were MRD-positive. All 2nd transplant donors were different from the 1st transplant donors. The conditioning regimens used in 2nd HSCT were busulphan-based (n=21), total body irradiation (TBI) (n=75) or melphalan-based (n=1). The 4-year overall survival (OS) and leukemia-free survival (LFS) were 52.64% (95%CI, 28.81-75.85%) and 49.86% (95%CI, 27.30-72.45%), respectively. The 4-year relapse incidence (RI) and non-relapse mortality (NRM) were 6.78% (95%CI, 3.12-14.77%) and 45.00% (95%CI, 26.13-77.50%), respectively. In univariate analysis, LFS was 39.47% (95%CI, 18.11-63.22%) and 68.54% (95%CI, 56.97-79.05%) (p=0.038) in patients who relapsed<6 months and ≥6 months after a 1st transplant. LFS was 66.25% (95%CI, 54.71-76.89%) and 40.00% (95%CI, 15.59-67.44) (p=0.0245) in patients whose CAR-T and 2nd HSCT intervals were ≤90 days (n=85) and >90 days (n=16), respectively. Whether patients had cytokine release syndrome (CRS) or not after CAR-T did not affect the outcomes of the 2nd HSCT.
Conclusions Our study shows that CAR-T therapy followed by consolidation second transplantation for B-ALL patients who had relapsed after a first HSCT could significantly improve long-term survival. The second transplantation could be considered in suitable patients and to be carried out within 90 days after CAR-T treatment. Reducing the intensity of the conditioning regimen should be explored to lower the NRM.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal